The healthcare landscape of 2026 is no longer just “incorporating” technology; it is being fundamentally rebuilt upon a foundation of artificial intelligence.
If 2024 was the year of experimentation and 2025 the year of pilot programs, 2026 is the year of integration. We have entered an era where AI is not a peripheral tool but a primary collaborator in clinical decision-making, drug discovery, and patient management.
Davos 2026: World Economic Forum white paper showcases Abu Dhabi as a global leader in intelligent healthcare
From “chatbots” to “clinical agents”
The most visible shift this year is the evolution of Generative AI from simple text-based assistants to Autonomous Clinical Agents. In early 2026, major Electronic Health Record (EHR) vendors like Oracle and athenahealth began rolling out native AI capabilities that do more than just summarize notes.
These agents now handle “agentic workflows” — meaning they can autonomously navigate the patient journey. For instance, if a patient presents with symptoms of a chronic condition, an AI agent doesn’t just record the data; it can proactively schedule the necessary diagnostic tests, flag potential anomalies in the results for the physician, and even draft the prior authorization paperwork for insurance companies before the doctor has even finished their rounds.
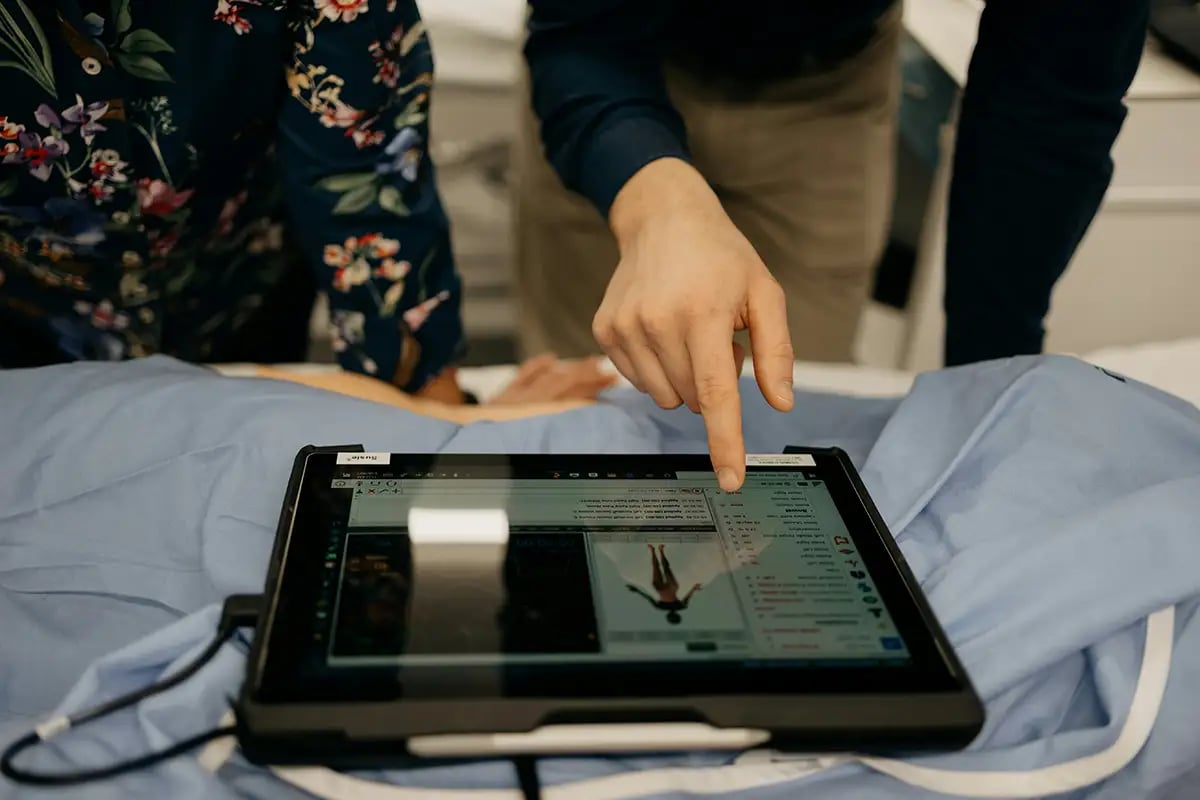
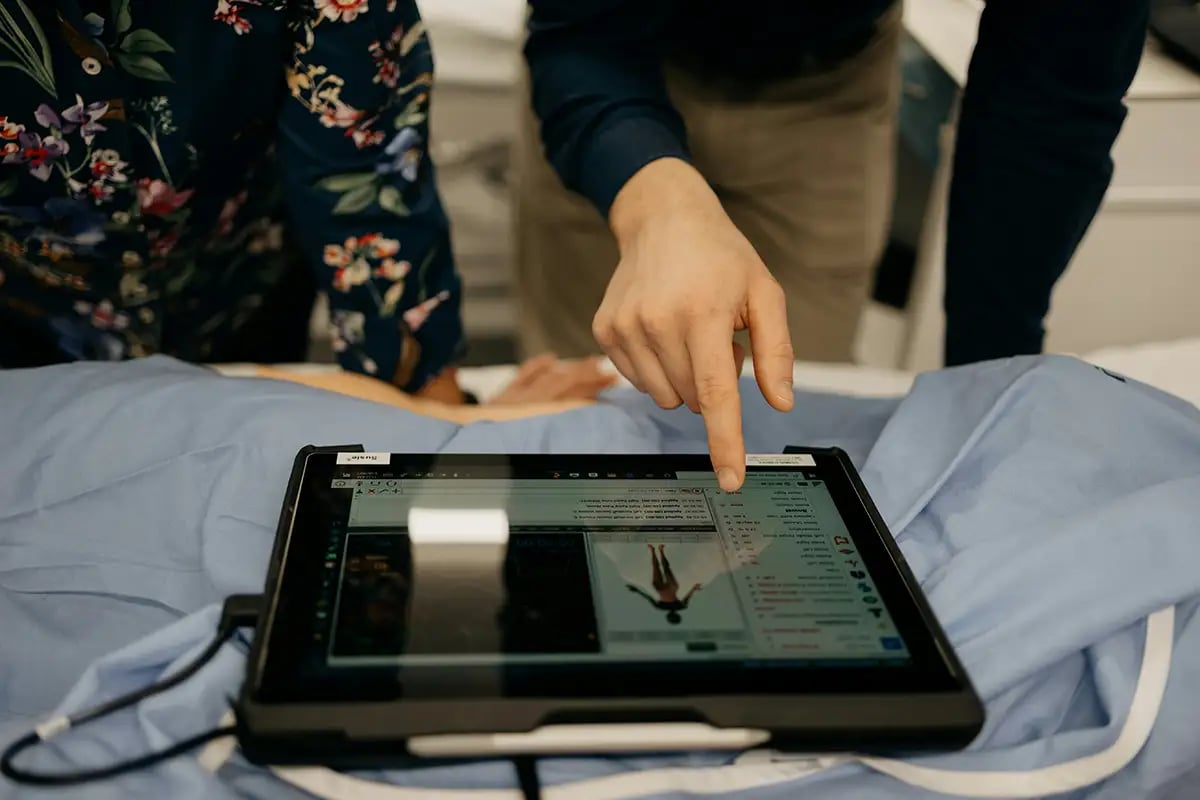
A recent study involving nationwide VA hospitals revealed that “Ambient Scribes” have become standard, leading to a 31 percent reduction in physician burnout. This improvement followed the implementation of tools that listen to consultations and automatically organize clinical notes, enabling doctors to maintain eye contact with patients instead of focusing on screens.
End of “trial and error” in drug discovery
The pharmaceutical industry has seen significant changes in drug discovery practices in 2026. Traditional approaches, which historically took over a decade and cost billions, are being supplemented and, in some cases, replaced by AI-supported molecular design.
In January 2026, NVIDIA and Eli Lilly announced a groundbreaking co-innovation lab built on the “Rubin” architecture, aimed at solving the “hardest problems” in biology. By utilizing “Physical AI”, researchers can simulate how a drug interacts with the human body at a molecular level before producing any physical samples.
Additionally, pharmaceutical giants have begun employing “Federated Learning” frameworks, which enable different companies to train their AI models on collective, industry-wide data while maintaining the confidentiality of sensitive proprietary secrets and raw patient data.
Furthermore, 2026 is notable for the transition of “Digital Twins” of patients from labs to clinical trials. These digital models allow researchers to test a drug’s efficacy on virtual representations of specific patients’ biology, significantly reducing the risk of adverse reactions during real-world trials.


Predicting diseases years early
We are witnessing a quantum leap in personalized care. As quantum computing begins to merge with AI, the ability to model complex protein folding and genetic mutations has reached unprecedented speeds.
In the U.K. and India, AI is being used to bridge the gap between traditional medicine and modern genomics. India’s recent launch of an AI-driven “Ayurgenomics” library catalogues indigenous medical texts to identify herbal formulations that can be cross-referenced with modern genetic data to treat modern diseases.
Meanwhile, AstraZeneca’s latest machine-learning models can now predict disease diagnoses years in advance by analyzing data from the U.K.’s massive health repository. These models can detect the early warning signs of over 1,000 different diseases, shifting the medical paradigm from reactive treatment to proactive prevention.
AI success meets reality
Despite the optimism surrounding AI advancements, 2026 has revealed sobering limitations regarding these technologies. As AI models grow more complex, the industry faces challenges such as “hallucinations” in clinical settings.
Microsoft’s MAI-DxO, for instance, boasts an impressive diagnostic accuracy of 85.5 percent in complex cases, significantly surpassing the average of just 20 percent for individual human physicians. However, some models continue to produce harmful recommendations in up to 22.2 percent of cases, primarily due to omissions of important information.
In response to these challenges, the FDA has introduced new “Predetermined Change Control Plans” (PCCPs), which require developers to demonstrate how their algorithms will evolve prior to any updates.
Sharon Klein, Partner and Co-Chair of privacy, security and data protection at law firm Blank Rome, notes that we are currently in a “perfect storm” where economic necessity is driving AI adoption faster than regulators can keep up.
The challenge for the remainder of 2026 will be creating a “patchwork” of global standards that ensure these “clinical copilots” remain safe and unbiased.


Restoring the human touch
The goal of AI in 2026 is not to replace the surgeon or the nurse, but to “amplify” them. By removing the “busy work” — the hours of charting, the manual data entry, and the administrative hurdles — AI is finally allowing healthcare professionals to return to the heart of their profession: Caring for the patient.
As we move through this year, the focus is shifting from “What can the AI do?” to “How can the AI help us do better?” The answer seems to be a future where the stethoscope and the silicon chip work in perfect harmony.
link

